Portosystemic Shunt in Dogs
What is a liver shunt?
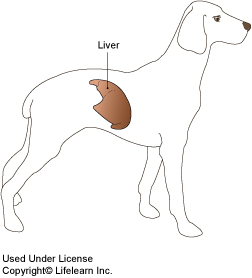
The portal vein is a large vein that collects blood from the gastrointestinal system, pancreas, and spleen and carries it into the liver, where toxins and other byproducts are removed. A liver shunt occurs when an abnormal connection persists or forms between the portal vein or one of its branches, and another vein, allowing blood to bypass, or shunt, around the liver.
In the majority of cases, a liver shunt is caused by a birth defect called a congenital portosystemic shunt. In some cases, multiple small shunts form because of severe liver disease such as cirrhosis. These are referred to as acquired portosystemic shunts.
How does a congenital portosystemic shunt develop?
All mammalian fetuses have a large shunt called the ductus venosus that carries blood quickly through the fetal liver to the heart. A congenital portosystemic shunt develops if:
- The ductus venosus fails to collapse at birth and remains intact and open after the fetus no longer needs it.
- A blood vessel outside the liver develops abnormally and remains open after the ductus venosus closes.
What are the clinical signs of a liver shunt?
The most common clinical signs include stunted growth, poor muscle development, abnormal behaviors such as disorientation, staring into space, circling or head pressing, and seizures. Less common symptoms include drinking or urinating too much, vomiting, and diarrhea. Dogs with a liver shunt often take a long time recovering from anesthesia. Behavioral clinical signs may only occur after eating high protein meals. Some dogs do not show signs until they are older, when they develop urinary problems such as recurrent kidney or bladder infections or stones.How is a liver shunt diagnosed?
Diagnosis is based on medical history and clinical signs. Common diagnostic tests include:
- Complete Blood Count (CBC) and Serum Chemistries. Typical abnormal findings include mild anemia or smaller than normal red blood cells (microcytosis), low blood urea nitrogen (BUN) and albumin, and increases in liver enzymes (AST, ALT).
- Urine may be dilute (low urine specific gravity) or there may be evidence of infection. The urine may contain small spiky crystals known as ammonium biurate crystals.
- Bile Acid Test. Most dogs with liver shunts have elevated bile acids. If the bile acids are mildly increased, or if the dog seems clinically normal despite abnormal test results, the tests will often be repeated in three to four weeks.
Additional diagnostic tests may include:
- Ultrasound with Doppler flow analysis.
- Computed tomography (CT) scan or nuclear scintigraphy which is a nuclear scan that measures blood flow through the liver).
- Portography which is an X-ray showing the blood vessels supplying and/or bypassing the liver, using radio-opaque dye injected directly into the portal vein.
- Magnetic resonance imaging (MRI).
- Exploratory surgery (laparotomy).
Certain breeds such as Yorkshire Terriers, Old English Sheepdogs, Irish Wolfhounds, Cairn Terriers, and Beagles have an increased incidence of portosystemic shunts. Small breed dogs usually have extrahepatic shunts (blood vessels outside of the liver) while larger breeds have intrahepatic shunts (abnormal blood vessels inside the liver). Extrahepatic shunts are less challenging to surgically repair than intrahepatic shunts.

What are bile acids?
Bile acids are produced in the liver and are stored in the gall bladder between meals. Normally, they are released into the intestines to help break down and absorb fats, after which they are reabsorbed by the portal system and enter the liver, where they are removed and stored again until needed. Dogs with liver shunts have increased bile acid concentrations in the blood because the liver does not get a chance to remove and store these chemicals after they are reabsorbed.
Tests that measure the amount of bile acids in the blood are used to screen for liver shunts. To perform this screening test, two samples are usually taken. The first sample is taken after fasting (pre-prandial). The second sample is usually taken two hours after being fed (post-prandial). The actual technique may vary based on the patient and on your veterinarian's preferences.
What is the treatment for a portosystemic shunt?
Dogs with portosystemic shunts are usually stabilized with special diets and medications, which attempt to reduce the amount of toxins that are produced and absorbed in the large intestines. Dogs that are severely ill may require intravenous fluids to stabilize blood sugar, an enema to remove intestinal toxins before they are absorbed and medications, such as diazepam (brand name Valium®) to stop seizures.
The most common medical treatment regime includes:
- Diet Change. The goal is to reduce the amount of protein in the diet and feed only high quality, highly digestible protein diets.
- Administering this sugar changes the pH in the large intestines, which decreases the absorption of ammonia and other toxins and makes the intestinal environment unfavorable for toxin-producing bacteria.
- In some cases, antibiotics are used to alter the bacterial population in the intestines, and to reduce intestinal bacterial overgrowth.
What is the prognosis?
If your veterinarian performs surgery before arthritis or other knee injury occurs, the prognosis is excellent. Your dog should regain full use of its leg. However, if arthritis has already developed in the knee joint, your dog may experience intermittent pain in the leg and the arthritis may progress. The higher the grade, of luxating patella, the higher the likelihood of reoccurrence postoperatively. Prescription anti-inflammatories, joint supplements, and/or special therapeutic joint diets may slow the progression of arthritis and help control any discomfort. Weight reduction is also recommended for pets that are overweight.
Consult with your veterinarian to determine the best post-operative plan for your pet.
What is the prognosis for a dog diagnosed with a portosystemic shunt?
Most dogs improve almost immediately with proper diet and medication. About one-third of the dogs treated medically will live a relatively long life. Unfortunately, over half of the dogs treated medically are euthanized within ten months of diagnosis because of uncontrollable neurological signs such as seizures, behavioral changes, or progressive liver damage. Dogs that tend to do well with long-term medical management are usually older at the time of diagnosis, have more normal blood test values and have less severe clinical signs.
Dogs with a single shunt, especially one that is extrahepatic, have an excellent prognosis if surgical correction is performed.
What does portosystemic shunt surgery involve?
Most surgeons use a device such as an ameroid constrictor that slowly closes the shunt. The ameroid constrictor is a metal band with an inner ring of casein, a protein found in milk. In the abdomen, the inner ring absorbs normal abdominal fluid and gradually swells, pressing on the shunt and encouraging it to scar shut. Shunts usually close within three to four weeks after ameroid constrictor placement.
Other surgical treatments include 1) cellophane bands that induce inflammation, gradually closing the shunt with scar tissue and 2) intravascular occlusive, clot-inducing devices.
How successful is surgical treatment?
Surgery provides the best chance for a long, healthy life in most dogs with extrahepatic shunts. If ameroid constrictor placement is performed, survival rate is over 95%. Many dogs are clinically normal within four to eight weeks following surgery. A small percentage of dogs will develop multiple acquired shunts and must be managed with a protein-restricted diet and lactulose for life.
What is involved in the post-surgical management of portosystemic shunt patients?
It is important to feed your dog a protein-restricted diet for minimum of six to eight weeks. After blood test values return to normal, your dog may return to a high-quality maintenance diet. Lactulose is usually given for several weeks after surgery.
The liver will begin to grow as the shunt closes and will often be normal size and function in two to four months. Blood tests will be repeated at regular intervals to evaluate liver function.


